Reading Time: 4 minutes
As healthcare workers treat new and growing emergencies, while simultaneously working to update legacy systems, it can be difficult to stay on top of existing patients’ health status. Especially if patients themselves aren’t proactive. Recurring appointments for health and wellness can be postponed or cancelled, and if no followup occurs to reschedule, this creates a gap in care.
EMRs and health records only tell part of the story. Today’s providers must piece together the bigger picture to understand how best to deliver care to patients and help them lead their healthiest lives.
But it isn’t always easy with systems that don’t talk to one another.
What are gaps in care?
Gaps in care, or care management, refers to the discrepancy between the care provided to patients and the recommended best practices in healthcare.
Gaps in care can manifest in several ways:
- A patient in an at-risk age group fails to comply with recommended screenings or preventative care (i.e., does not get a yearly mammogram, blood pressure screening, or misses a vaccine booster)
- A patient’s new diagnosis is not shared with their PCP or specialist for another related condition
- A patient can’t schedule a behavioral health appointment in a timely fashion and leaves for another provider
- A patient does not follow recommended prescription guidelines for a chronic condition
- A child who is not scheduled for regular well visits or vaccinations
- A patient is not able to find the care they need in their network or area
And it’s not just important for your patients. It’s important for your bottom line, too. An 8% conversion rate across two gaps in care has the potential to deliver $15.7MM in incremental revenue (which can be put toward improving processes, outreach programs, and more):
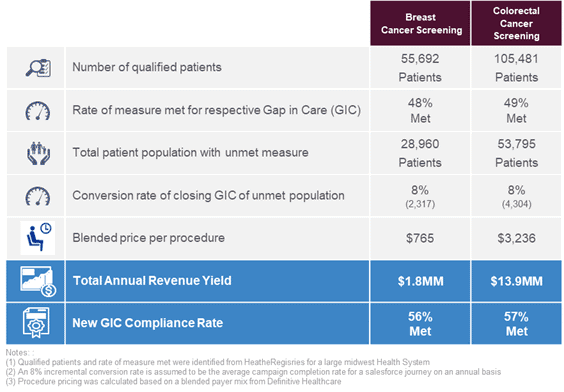 Data from Cerner and Definitive Health
Data from Cerner and Definitive Health
Closing gaps in care starts with understanding your patients
Effective patient engagement that helps reduce gaps in care requires more than just knowing the patient’s medical history. But the challenge is that a gap in care is just that — a gap.
Providers must ask themselves:
- How do we identify patients with a potential gap in care and then confirm the gap exists?
- How do we engage the patient to close the care gap and follow through to make sure it is closed?
It also requires knowing – at an individual level – their tolerance for an in-person visit, their means for engaging with a telehealth option (if available), access to transportation and other social determinants of health, current health condition, and other risk factors.
You need to know the different types of patients that are coming into your organization. You want to figure out:
- What are the most relevant needs of your patients?
- What are their communication and care preferences?
- How do they want to engage with you?
- What information do you already know about them?
- What are their specific social determinants and needs
To be able to craft the best possible patient experience and close gaps in care, you first have to know more about your patients.
Creating a holistic patient profile
Creating a holistic patient profile to gather info from the patient and display known demographic information that can be verified and updated as needed. This allows for the assignment to a work queue and creates a path for closing the case. It also means that anytime a patient engages with you, you have a complete picture of their health — including risk factors, social determinants, and medical history — so you can provide better care.
But knowing all this still does not bring the patient into the clinic or the doctor’s office.
There is also the matter of maximizing appointment scheduling. Will a text directly from a provider that notifies a patient of a gap in care result in a confirmed appointment better than an email or call? Can you offer a day and time that works best with the member’s schedule? Creating a relationship with the patient to drive better health outcomes requires having every conceivable piece of consumer data in one place.
By building out journeys for your patient personas, you can close gaps in care, establishing robust preventative routines that ultimately help your patients stay as healthy as possible for as long as possible. Engaging consumers and patients where they are builds trust and confidence that keeps patients in the system and encourages them to refer their friends and family to your practice.
A 360-degree view of your patients, along with streamlined patient journeys with Salesforce, can provide you with a full understanding of a patient, ensuring that your healthcare team always engage in the right channel, at the right time and with the right content or message – at every point in the individual’s healthcare journey.
Case study: what solving gaps in care looks like in action
Silverline partnered with a leading Midwest hospital to close gaps in care, improve quality of services offered, and digitally transform their operations. The provider was already using Cerner to collate data from payers, doctors’ offices, their EHR, and health information exchanges.
Adding a clinically informed CRM took that data and delivered the right content at the right time, to the right person, via the right channel. They worked with Silverline to combine Cerner’s HealtheIntent® and HealtheCRMSM and Health Cloud and Marketing Cloud technology from Salesforce to enhance their consumer and provider engagement.

Integrating CRMs and EHRs together maximize the benefits of both platforms. The transition to patient-centric healthcare has made every interaction between a patient and your organization critical. CRM allows you to take full advantage of your data to tailor your external messaging strategies, outreach centers, and overall patient experience.
These components provide the framework for identifying care gaps for patients, creating actionable records in Health Cloud, and automating engagement to close the care gap. The algorithms already built into the Cerner HealtheIntent® product define what the measure is for breast cancer screening and when a patient comes due, for example. Now, the team can use one source of truth to define care gaps and close them.
See how Silverline’s healthcare experts can help you solve gaps in care. Learn more.