The term utilization management (UM) is nothing new — it’s been in our vocabulary since the 1970s — but it’s become an increasingly important term as a means of medical cost management. Overutilization and waste of resources, in combination with increased healthcare costs, put pressure on health insurers (payers) and employers to keep premiums down for the fully insured and claims trends down for the self-insured.
What began as a simple check-the-box before hospital stays grew to today’s complex utilization review process, which entails a prospective review (prior to treatment), concurrent review (during treatment), and retrospective review (after treatment).
So how can payers modernize a process that began decades ago, address siloed UM systems, and accommodate a single source of truth for care management, providers, members, and customer service?
Salesforce Health Cloud is here to help.
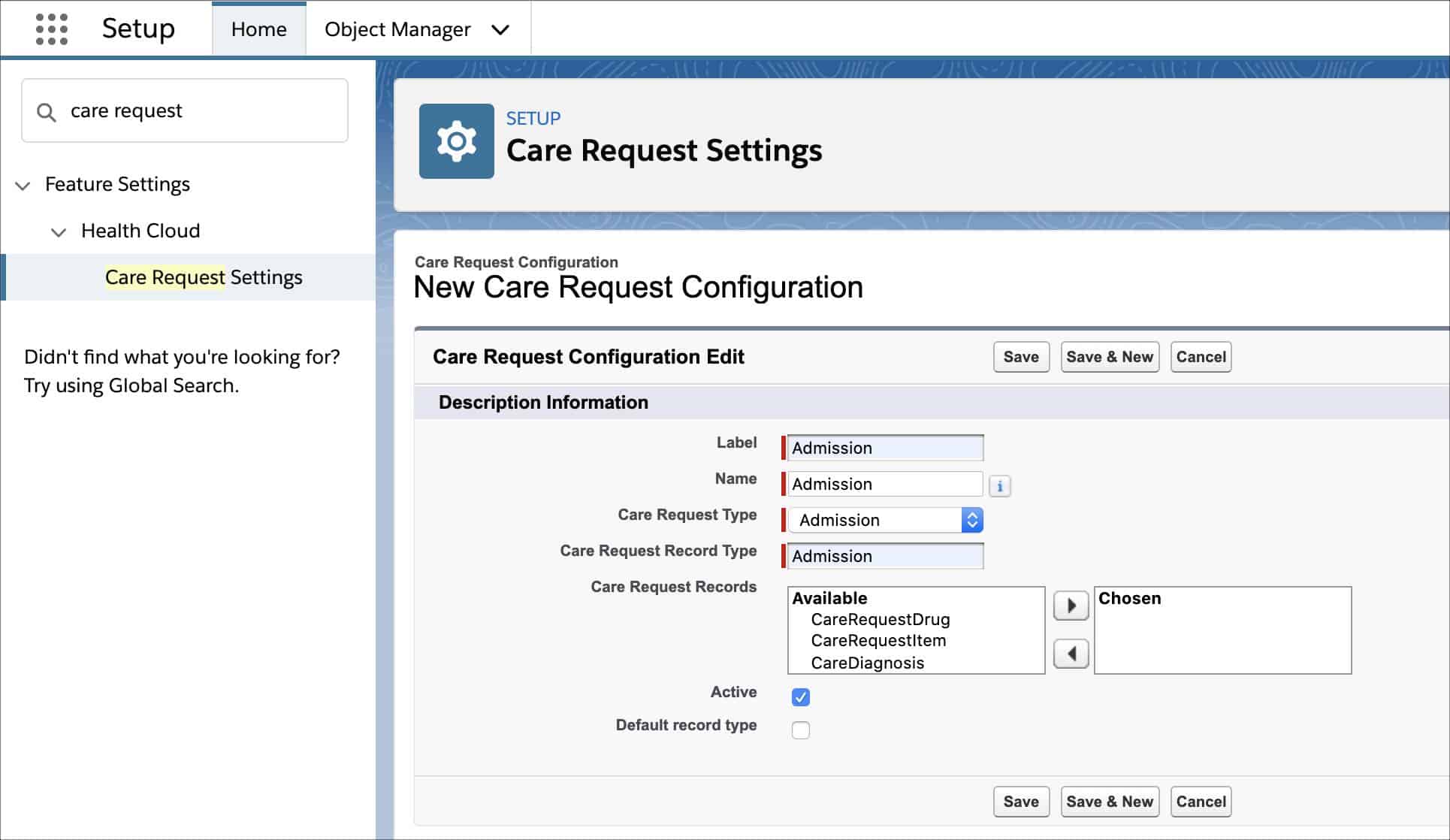
Salesforce Health Cloud manages care requests
Payers can manage precertification and prior authorization using the Care Request feature within Health Cloud.
The Care Request model within Health Cloud supports payer utilization management processes such as: prescription drug preauthorizations, service preauthorizations, and admissions review so that each stakeholder can access the data they need to make a decision — and most importantly, help patients get the care they need.
1. For the care management team
Silverline works with payers to perform utilization management services within Health Cloud or integrate Health Cloud with their existing utilization management system. This might be taking requests via a provider portal (see below) or directly within your existing system.
With Health Cloud, the care management team can:
- Easily view requests within designated list views
- Identify standard vs. expedited requests quickly
- See status updates and new requests up front
- Appropriately manage their workflow based on line of business or service level agreements
- Prioritize authorization requests, escalating them to a director for review if needed
- Get additional information from providers without needing to make a phone call or use another system
Everything you need for authorization requests is easily accessible to every member of the care management team in one place, and Silverline can configure Health Cloud to provide instant notification to the member, provider, and facility (if applicable) of the decision.
2. For providers
One easy way for providers to get the information they need is by creating a provider portal that houses all of their authorization workflows. Silverline can create a Salesforce Experience Cloud portal for providers participating in a payer’s network.
This portal provides several areas of functionality; however, performing prior authorization requests is one of the most critical. As mentioned above, prior authorization requests can begin within the provider portal, where the provider has the ability to confirm those services for the member and submit the authorizations accordingly.
With a streamlined, easy-to-use interface, a provider portal can:
- Make it easy for providers to attach necessary documentation and provide commentary
- Track the progress of authorization within the portal
- Submit additional documentation as needed
- Void the authorization if no longer required
Providers no longer need to bombard the payer with faxes or phone calls hoping that the authorization is quickly reviewed by the payer. It can all happen with instant notifications and digital communication, making the process smooth for everyone.
3. For members
Similar to the provider portal described above, Silverline can create a member portal in which members would have immediate access to the status of their prior authorization request.
Transparency of the steps within the process allows the member the peace of mind of knowing that their doctor appropriately requested approval for the necessary service and that the service is being reviewed for medical necessity. Members no longer need to wait to hear from their doctor or health plan that their authorization has been approved or denied.
4. For customer service representatives
Customer service often faces the “swivel chair” effect of too many systems and logins, causing dead airtime or long waits for members and providers looking for answers.
With Salesforce Health Cloud, members can feel confident that when they call into customer service, the agent will be able to quickly access the status of their authorization within the Health Cloud console. If questions persist, the agent can quickly alert the care management team or the provider utilizing the features of Health Cloud.
How Silverline can help
At Silverline, we have the payer expertise to provide solutions to payers facing the above challenges. We understand these challenges and have extensive experience solving these challenges for our clients. We use the full suite of Salesforce products to assist our clients with:
- Maximizing authorizations for their members
- Creating member services solutions that deliver immediate value for member populations
- Gathering unique, actionable insights from the data captured by payers
Silverline offers payers a blueprint for success in which every functional area within your organization can benefit from our industry knowledge, best practices, and thoughtful consultation. Learn more about how we can help your organization.