Silverline believes in taking a patient journey approach to Weight Loss/Bariatric Surgery. Weight Loss/Bariatric Surgery is a growing use case within healthcare organizations as the US population struggles with obesity. Weight loss has significant health benefits and can reduce or eliminate the impact of multiple chronic diseases including diabetes, hypertension, high cholesterol, obstructive sleep apnea, and joint pain.
The journey may start with a morbid obesity diagnosis, but often times it starts with a person being motivated to change their life because obesity is affecting their family life and career. It starts with educating the patient about their treatment options, both surgical and non-surgical, then set course for a healthier and happier life.
Patients should not feel like they have to navigate weight loss surgery alone, but rather have a nurse navigator and a care team, someone with access to all of the resources needed to make the journey as efficient and effective as possible to hold their hand every step of the way.
Patient Acquisition
- One key to a successful program is identifying candidates and enrolling them in a Health Cloud Care Management Pathway. This pathway allows for early intervention to overcome objections and barriers to care while qualifying the patient for the bariatric surgery.
- Getting the patient to attend a seminar and committed to the next steps is critical.
- Integration of Marketing Cloud allows for engagement tracking and targeted marketing efforts to ensure candidate patients are knowledgeable about the qualification process, the commitment required, clearance process and dietary changes required.
- Understanding a patient’s clinical touchpoints during their patient journey allows for synchronized Marketing Cloud and Health Cloud status updates, gathering of information, and notifications for both the patient and the care team.
Provider Network Management
- Defining and building provider and facility profiles allow for the seamless navigation of bariatric patients throughout the system, ensuring that patients are referred within the network and all unique attributes of their journey (barriers to care, support system, care team, etc.) are shared with the team.
- This includes defining those ancillary care team members including dieticians, social workers, and community-based resources.
- At a minimum, your application should allow for tracking engagement, marketing and educational efforts with your care team members.
- If possible, scheduling should be consolidated in the application to provide a seamless patient navigation experience for the nurse navigator and/or non-clinical patient navigators.
Care Navigation
- As bariatric surgery has transitioned from experimental/cash pay to mainstream/covered by insurance, creating continuity of care and keeping the patient loyal throughout the process is challenging.
- While there are several different types of procedures, all surgery candidates go through a detailed qualification process:
- Meet insurance criteria
- Psychological evaluation
- Labs and Imaging
- Diet and exercise modification
- Pulmonary, GI and Cardiac clearance
- Referral Coordinators would manage the myriad of testing and clearances required. Patients need to report weight, diet, and exercise while completing assigned tasks.
- Care Coordinators would manage the overall process while Dieticians would have regular interactions with the patient.
There is also a significant post-procedure follow-up protocol with specific milestones to be achieved.
- Weekly follow-up for the 1st 4 weeks consisting of office visits, dietary intake assessments, nutritional counseling and collection of anthropometrics
- Monthly follow-ups to include assessments, lab testing, and regular check-ins with the care team
- 6-month Follow-up including During the six-month visit, anthropometrics will be measured (body mass index, body weight, fat mass, and fat-free mass), and quality of life status and eating behaviors may be determined from standardized questionnaires. Furthermore, you will have dietary assessments and may be seen by nutrition or exercise professionals. Consultations with the behavioral health provider are optional and available.
Patient Navigation Tool
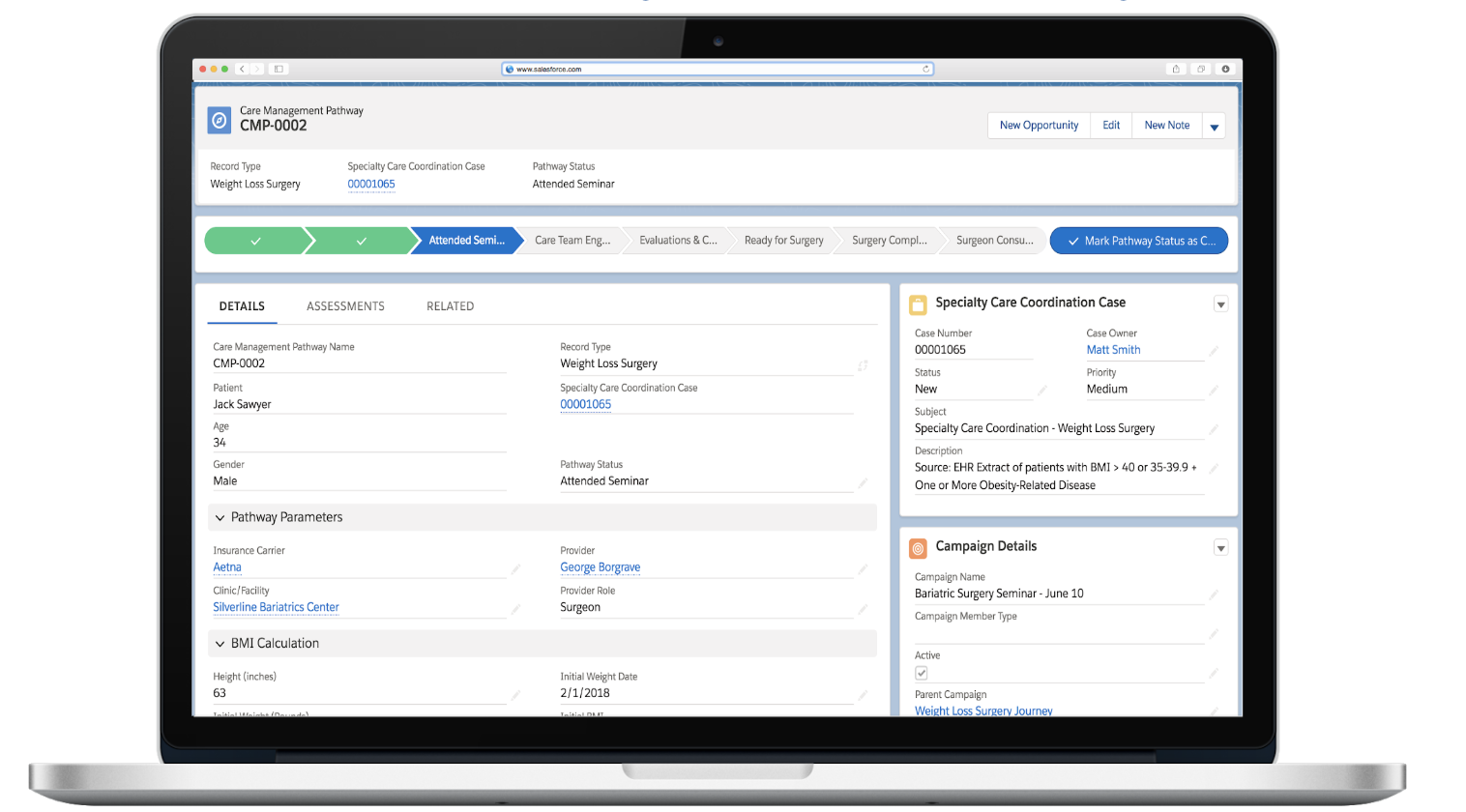
Choosing the right software application for service line navigation is essential to the success of a bariatric surgery program. Silverline has created a Care Management Pathway on Health Cloud that serves as the driving record for patient journeys like bariatric surgery. It is customizable for healthcare organizations and other patient journey use cases and is integrated to Marketing Cloud for coordinating patient engagement between the patient/caregiver and the care team. It also includes assessments, services, knowledge articles, provider search, and appointment scheduling. These components provide the framework for navigating patients on a journey from suspected cancer to recovery/remission or hospice.
Silverline can help organizations build the tools to provide care navigation for bariatric patients, as well as, manage referrals, perform nurse triage, manage a provider network, manage a risk-based population and much more. Wherever you start, Silverline has the tools and the experience to help you be successful.
To learn more about Silverline’s Healthcare Expertise, contact us today.




